Prion expert sorts through pieces of the protein puzzle
Prions are almost as much of a mystery now as they were 20 years ago when scientists began studying them in earnest— around the time that mad cow disease surfaced in Great Britain. In 2001, DMS assembled its own team of prion researchers—led by biochemist Surachai Supattapone, M.D., Ph.D., who had worked for six years in the lab of prion guru Stanley Prusiner, M.D., winner of the 1997 Nobel Prize. Supattapone's team has been taking a biochemical approach to unraveling the prion mystery and reported some recent findings in the journal Biochemistry.
Prion proteins are thought to be responsible for causing mad cow disease and several other fatal brain diseases called transmissible spongiform encephalopathies (TSEs). TSEs leave the brain riddled with Swiss-cheeselike holes. Such neurodegenerative diseases—there are inherited, sporadic forms and infectious forms—are rare but frightening. People and animals who are stricken lose all control of their bodies, descend into dementia, and finally die.
|
|
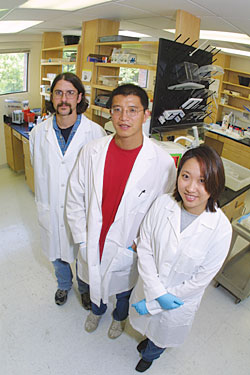
Surachai Supattapone, center, and his collaborators—Nathan
Deleault, left, and Koren Nishina, right—have been taking
a biochemical approach to the puzzle of prion diseases. |
Hypothesis: "Prusiner's hypothesis is that the TSE infectious agent was not a virus but rather a protein," Supattapone says. A normal mammalian brain protein, called PrPC, misfolds into the infectious form of the prion protein, called PrPSc. The Pr- PScs accumulate to form plaques in the brain. "Normal PrPC changes shape to become infectious, and this process is catalyzed by the PrPSc," says Supattapone. Until Prusiner's discovery, no one was aware of any infectious agent that did not contain genetic material.
Cows: Prion diseases have been around for at least 300 years, first as scrapie, which occurred in sheep initially and is now known to also occur in humans, deer, elk, mink, rats, mice, hamsters, possibly monkeys, and, of course, cattle. In fact, the appearance of bovine spongiform encephalopathy (the scientific name for mad cow disease) in Great Britain in the mid-1980s was thought to be linked to cattle feed that included ground-up sheep bones, some of which may have been from scrapie-infected sheep.
Although mad cow disease seemed to disappear once the practice of adding sheep products to cattle feed was stopped, it resurfaced recently and is now spreading throughout Europe. A few people in Great Britain have died from its human form— Creutzfeldt-Jakob disease—apparently as a result of eating infected beef.
Diseases don't usually jump from one species to another, but scientists have found that spongiform encephalopathies can be transmitted between species. Mice injected with TSE-infected brain tissue from cows will usually contract the fatal disease within a year.
No one understands the exact mechanism for this, but Supattapone hopes to shed new light on the process. He's using a biochemical approach to studying how PrPC converts into PrPSc in a test tube. "We found that chemicals that block disulfide formation [also] block the formation of PrPSc," he explains.
"This is the first discovery that the formation of PrPSc requires a reactive chemical group."
S&H: These chemicals— called sulfhydryl groups—are made of sulfur and hydrogen (S and H) molecules. In nature, their chemical bonds can break and reform, so two S-H molecules could break apart and the two sulfur molecules would form a disulfide bond, or S-S.
"My analogy for this is hair," Supattapone explains. "Hair has a lot of free sulfhydryl groups." Over a few weeks' time, the S-H groups break apart and reform as S-S bonds, and "the hair becomes very coarse. That's the disulfide bonds coming together. Then you come in with your hair conditioner, which contains a chemical that reduces the disulfide bonds back to free S-H, so your hair becomes soft again."
Likewise, the chemicals used in Supattapone's experiments interfere with the formation of disulfide bonds. "It is a clue that there may be a cofactor containing the free sulfhydryl group, such as an enzyme that helps to catalyze the process of forming PrPSc from PrPC," he says. The team has another paper coming out soon, in the journal Nature. Therapeutic strategy: The work may be a first step in finding a therapeutic strategy against prion diseases. "This is simpler than a virus," Supattapone says. Viruses can evolve to be resistant to treatment, but prions can't. "So if we could interfere, we could actually stop it forever."
Laura Stephenson Carter
If you would like to offer any feedback about this article, we would welcome getting your comments at DartMed@Dartmouth.edu.
